About eating disorders
What are eating disorders?
Eating disorders are a range of conditions that can affect someone physically, psychologically and socially, regardless of gender, age or size. A person with an eating disorder may focus excessively on their weight and shape, leading them to make unhealthy choices about food with damaging results to their health.
Although serious, eating disorders are treatable conditions and full recovery is possible. The sooner someone gets the treatment they need, the more likely they are to make a full recovery. Eating disorders are complex; there’s no single cause and not all symptoms will apply to all people.
Anorexia Nervosa and Bulimia Nervosa are the most commonly spoke about eating disorders. However, there are several types of eating disorders and all of them are important.
Some of the main eating disorders are as follows:
People who have anorexia try to keep their weight as low as possible by not eating enough food or exercising too much, or both. This can make them very ill because they start to starve. They often have a distorted image of their bodies, thinking they are fat even when they are underweight. Men and women of any age can get anorexia, but it's most common in young women and typically starts in the mid-teens.
People who have bulimia go through periods where they eat a lot of food in a very short amount of time (binge eating) and then make themselves sick, use laxatives (medication to help them go to the toilet) or do excessive exercise, or a combination of these, to try to stop themselves gaining weight. Men and women of any age can get bulimia, but it's most common in young women and typically starts in the mid to late teens.
Binge eating disorder involves regularly eating large portions of food all at once until you feel uncomfortably full, and then often upset or guilty. Binges are often planned in advance and the person may buy "special" binge foods. Men and women of any age can get binge eating disorder, but it typically starts in the late teens or early 20s.
It is currently not recognised in a clinical setting as a separate eating disorder, so you would not be officially diagnosed with “orthorexia” at the doctors, but the term would likely be brought up in discussion. Orthorexia refers to an unhealthy obsession with eating “pure” food. Food considered “pure” or “impure” can vary from person to person. This doesn’t mean that anyone who subscribes to a healthy eating plan or diet is suffering from orthorexia. As with other eating disorders, the eating behaviour involved – “healthy” or “clean” eating in this case – is used to cope with negative thoughts and feelings, or to feel in control. Someone using food in this way might feel extremely anxious or guilty if they eat food they feel is unhealthy.
- Other Specified Feeding or Eating Disorder (OSFED) -
It is common for symptoms to not fit with the exact diagnostic criteria for anorexia, bulimia, or binge eating disorder, so it is classed as an OSFED – OSFED accounts for a large percentage of eating disorders.
Examples of OSFED's are:
- Atypical anorexia – where someone has all the symptoms a doctor looks for to diagnose anorexia, except their weight remains within a “normal” range.
- Bulimia nervosa (of low frequency and/or limited duration) – where someone has all of the symptoms of bulimia, except the binge/purge cycles don’t happen as often or over as long a period of time as doctors would expect.
- Binge eating disorder (of low frequency and/or limited duration) – where someone has all of the symptoms of binge eating disorder, except the binges don’t happen as often or over as long a period of time as doctors would expect.
- Purging disorder – where someone purges, for example by being sick or using laxatives, to affect their weight or shape, but this isn’t as part of binge/purge cycles.
- Night eating syndrome – where someone repeatedly eats at night, either after waking up from sleep, or by eating a lot of food after their evening meal.
Eating disorders do not always involve the physical aspect of being thin, someone with a normal or high BMI may still have an eating disorder; you just may not be able to see it. If you or someone you know could be suffering with an eating disorder, it is important to get help. You can always go to your GP who can pass you on to services and people who can give you support and advice.
The Centre for Clinical Interventions has several resources available for self help and help for others struggling with an eating disorder along with helpful guidance with other mental health challenges.
Who can help?
If you are worried that you may have an eating disorder, visit your GP for support and access the following websites for more information:
- Beat – Beat provides Helplines for people of all ages, offering support and information about eating disorders no matter where you are in your journey. These Helplines are free to call from all phones.
Our Helplines are open 365 days a year from 1pm – 9pm during the week, and 5pm–9pm on weekends and bank holidays. Support on the Helpline is available by phone, email, webchat (live link) through our social media accounts and by letter. Calls to the helpline are free from landlines and mobile phones within the UK and do not appear on itemised bills.
Sometimes our lines are busy. If you can't get through immediately, please do try again or try our one-to-one web chat or send us an email.
If you are in need of urgent help or medical advice for yourself or someone else, please contact 999 or the Samaritans on 116 123 if you or someone else is in immediate danger. If you are looking for medical advice, contact your GP or 111.
Helpline for England: 0808 801 0677
Helpline for Scotland: 0808 801 0432
Helpline for Wales: 0808 801 0433
Helpline for Northern Ireland: 08088 010 434
- Personalised Eating Disorder Support (PEDS)- (Self-Refer) - offers assessment and support with signposting and where appropriate to service users, families and loved ones and professionals. We offer our service users individual sessions which are tailored to meet the unique needs of each person. We also provide family sessions which include practical help, education and support. We operate mostly remotely and sessions are via Microsoft Teams or Zoom. This includes assessments, 1:1s and groups (service users and carers). Face-to-face sessions, if required, are held at Boroughbury Medical Centre
- SEED - We are a group of ordinary people with first hand experience of eating disorders, who make a difference to those people whose lives are blighted by this devastating illness. All services can be accessed through self-referral. We provide support and services for people living in Hull East Riding and Out of Area.
- MaleVoicED - MaleVoicED is a charity providing a platform to all males enabling the sharing of narrative around poor relationships with food and co-morbid conditions. MaleVoicED also shares the experiences of caregivers, friends and associates who have been affected by such poor food related relationships. MaleVoicED hopes that with the sharing of such narratives, services for males will be improved.
- Overeaters Anonymous - Overeaters Anonymous is a fellowship of individuals who, through shared experience, strength and hope are recovering from compulsive overeating. Welcomes everyone who wants to stop eating compulsively.
- British Nutrition Foundation - Promotes the wellbeing of society through the impartial interpretation and effective dissemination of scientifically based knowledge and advice on the relationship between diet, physical activity and health.
- Recover Your Life - One of the biggest and best Self Harm Support Communities on the Internet, offers help on a variety of topics surrounding self harm, including self injury, eating disorders, mental health issues, abuse and bullying, as well as drugs and alcohol and first aid.
- The Mix - The Mix is a website for young adults. It has advice and will help you take on any challenge you’re facing - from mental health, eating disorders to money, from homelessness to finding a job, from break-ups to drugs. Talk to them via online, social or their free confidential helpline.
Mental health challenges are common but help is available and with the right support many people recover completely. Check out our Support Services Page for lots of services who are local and national!
*Some information gathered from www.nhs.uk and the services listed.
Signs and symptoms
You may not feel you relate to any of the below. You could still be struggling and should access help. Eating disorders are not gender specific and can happen to anyone at any age.
Symptoms of general eating disorders include:
To view general signs and symptoms please click here.+
- Spending a lot of time worrying about your weight and body shape
- Avoiding socialising when you think food will be involved
- Changes in eating habits and routines
- Going to the bathroom after eating and making yourself sick, taking laxatives after you eat and/or exercising more than usual
- Exercising too much
- Fascination of food
- Physical symptoms could include, feeling cold, tired, or dizzy, pains, tingling or numbness in your arms and legs (poor circulation), feeling your heart racing, feeling faint – sign post to more physical symptoms
- Problems with your digestion, such as bloating, constipation or diarrhoea
- Not getting your period or other delayed signs of puberty
- Changes in weight
- Lying about how much you have eaten, when you have eaten, or your weight
- Wearing loose or baggy clothes to hide their weight and or body
- Not wanting to be kind to yourself, including self-care, general hygiene, sleep, nutrients and treating yourself
- Socially withdrawn and isolated
- Changes in mood, this could include feeling anxious or depressed
- Low confidence and self-esteem
- Feeling out of control around food
https://www.nhs.uk/mental-health/feelings-symptoms-behaviours/behaviours/eating-disorders/overview/
Early habits - There can be early signs or habits that are unhealthy for individuals to do. It is a good idea to act quickly. Beat have a 'Know the first signs' poster which you can see to the right or you can download a copy here.
Physical symptoms include but are not limited to:
Tiredness and fatigue, cold skin, sight and eye health issues, weak bones, hair loss, lanugo – fluffy light hair growth, behavioural changes and mood swings, abusing laxatives, low self-esteem, poor nail growth, low concentration, sleeping patterns being disturbed, irritability, feeding others, depression and anxiety, disappearing after mealtimes, poor teeth, skin condition changes, changes to menstrual cycles, dizziness, nose bleeds, anaemia, creating or following rules around food, excessive exercising (even when ill), hyper-vigilant/on edge.
The above signs and symptoms are across most eating disorders. This list is not inclusive, you may find that what you are experiencing is different from this and are still concerned. You may also find that you are experiencing symptoms across several eating disorders.
Individual experiences of eating disorders may vary. You may not identify with the below definitions or find that you connect with more than one definition.
For more information on:
Anorexia
The NHS defines Anorexia as 'An eating disorder and serious mental health condition. People who have Anorexia try to keep their weight as low as possible by controlling their intake of food through not eating enough food or exercising too much, or both. This can make them very ill because they start to starve. People may often have a distorted image of their bodies' (NHS, 2021).
Sometimes the goal is not to reduce or have a low weight, but our weight is affected as a result of the illness. You can still be diagnosed with Anorexia but not be medically classed as underweight.
Links to more information:
https://www.nhs.uk/mental-health/conditions/anorexia/overview/
https://www.beateatingdisorders.org.uk/types/anorexia
.
Binge Eating
The NHS defines Binge Eating Disorder as the following 'Binge eating disorder involves regularly eating a lot of food over a period of time until you're uncomfortably full. Binges are often planned in advance, usually done alone, and may include "special" binge foods. You may feel guilty or ashamed after binge eating' (NHS, 2020). You may feel out of control and unable to stop.
Links to more information:
https://www.nhs.uk/mental-health/conditions/binge-eating/overview/
https://www.beateatingdisorders.org.uk/types/binge-eating-disorder
.
Bulimia
The NHS defines Bulimia as 'An eating disorder and mental health condition. People who have bulimia go through periods where they eat excessive amounts of food (binge eating) and then make up for this by purging what they have eaten e.g. by making themselves sick, using laxatives (medicine to help them go to the bathroom) or doing excessive exercise, or a combination of these, to try to stop themselves gaining weight.' (NHS, 2020).
Links to more information:
https://www.nhs.uk/mental-health/conditions/bulimia/overview/
https://www.beateatingdisorders.org.uk/types/bulimia
.
Diabulimia
Diabetes UK define Diabulimia as 'An eating disorder that only affects people with Type 1 diabetes. It’s when someone reduces or stops taking their insulin to lose weight. But when you have Type 1 diabetes, you need insulin to live. So without it, there can be life-threatening consequences' (Diabetes UK).
Links to more information:
https://www.diabetes.org.uk/guide-to-diabetes/life-with-diabetes/diabulimia
https://www.nationaleatingdisorders.org/diabulimia-5
..
Avoidant/Restrictive Food Intake Disorder (ARFID)
BEAT define ARFID as 'A condition characterised by the person avoiding certain foods or types of food, having restricted intake' (BEAT, 2019). A person will avoid certain types of food by drastically reducing their intake. People may do this for a number of different reasons, for example disliking certain textures, tastes or smells, having a distressing experience around food or being unable to identify when you are hungry.
Links to more information:
https://www.beateatingdisorders.org.uk/types/arfid
https://www.nationaleatingdisorders.org/learn/by-eating-disorder/arfid
https://www.arfidawarenessuk.org/copy-of-what-is-arfid-1
.
Other Specified Feeding or Eating Disorder (OSFED) also known as Eating Disorders Not Otherwise Specified (EDNOS)
BEAT define OSFED as when a person’s symptoms don’t exactly fit the expected diagnosis for any of these three specific eating disorders - Anorexia, Bulimia, and Binge Eating Disorder. They may have symptoms from a variety of different eating disorders. In that case, they might be diagnosed with an 'Other Specified Feeding or Eating Disorder' (OSFED) (BEAT, 2020).
Links to more information:
https://www.beateatingdisorders.org.uk/types/osfed
https://www.nationaleatingdisorders.org/learn/by-eating-disorder/osfed
.
Orthorexia
BEAT define Orthorexia as 'An unhealthy obsession with eating “pure” or clean food. Food considered to be “pure” or “impure” can vary from person to person. This person may then only consider eating foods they consider to be clean, cutting out other groups of food completely, for example refined sugars or processed foods etc. It is not currently recognised in a clinical setting as a separate eating disorder, so someone who visited the doctor with the symptoms would not be officially diagnosed with “orthorexia”, although the term may be brought up when discussing their illness' (BEAT, 2020). This can become an unhealthy and unbalanced diet due to missing key nutrition and vitamins that comes with a balanced diet.
Links to more information:
https://www.beateatingdisorders.org.uk/types/orthorexia
https://www.nationaleatingdisorders.org/learn/by-eating-disorder/other/orthorexia
.
Rumination Disorder
BEAT define Rumination disorder as 'An illness that involves repetitive, habitual bringing up of food that might be partly digested. It often occurs effortlessly and painlessly and is not associated with nausea or disgust' (BEAT, 2019).
Links to more information:
https://www.beateatingdisorders.org.uk/types/rumination-disorder
https://www.nationaleatingdisorders.org/rumination-disorder
.
Pica
BEAT define Pica as 'A feeding disorder in which someone eats non-food substances that have no nutritional value, such as paper, soap, paint, chalk, or ice. For a diagnosis of pica, the behaviour must be present for at least one month, not part of a cultural practice, and developmentally inappropriate' (BEAT, 2020).
Links to more information:
https://www.beateatingdisorders.org.uk/types/pica
https://www.nationaleatingdisorders.org/learn/by-eating-disorder/other/pica
.
Bigorexia/Muscle Dysmorphia
Body Dysmorphia Disorder (BDD) Foundation, describe Muscle Dysmorphia 'As sometimes used to describe BDD in which the person is preoccupied with muscle size, shape and leanness. People with muscle dysmorphia often believe that they look small, when in reality they look normal or may even be more muscular than average' (Body Dysmorphia Disorder Foundation).
Links to more information:
More about BDD – BDDF (bddfoundation.org)
https://www.verywellmind.com/bigorexia-muscular-dysmorphia-reverse-anorexia-2328475
Bigorexia: Never Buff Enough | BBC Newsbeat - YouTube
If you're living with an eating disorder
Disclaimer - The information on this website is not absolute. It has been created by individuals who have experienced eating disorders and from their observations of their journey through recovery, so some of the text may not resonate with you. The information on this page may be triggering. If you need urgent mental health crisis support, call NHS111 Option 2.
Contents:
.
Warm words
Welcome to our page.
Are you currently facing challenges surrounding eating, your relationship with yourself and your body? This website has been put together by those who have experienced different eating challenges and recovered or in recovery. We want you to know you are not alone and support is available.
.
Words of encouragement
- You matter and your feelings are valid
- You are not the eating disorder; you are still yourself

- You are loved and will always be loved
- You have top-notch qualities, don’t forget about them
- Recovery is possible and there is life after an eating disorder. You can write down your reasons to recover
- Stay connected with your support network
- Reach out. You are worthy of help
- Talk to yourself as you would to someone you love
- There are times of joy beyond the eating disorder
- Each day is a new day
- Small steps are still progress
- Be proud of yourself for how far you have come
- You can still be a friend, partner, employee
- People will listen
- There is no one or reason to blame
- Find reasons to love yourself
- Small steps are still progress, celebrate them
- Every journey is different, but the end goal is the same
- Your eating disorder doesn’t have to fit in a specific box
- It’s ok to speak out, don’t be ashamed, your mind wants to silence you. You wouldn’t be ashamed of breaking your leg
- Forgive yourself
.bBack to top/menu
Explaining eating disorders
‘An eating disorder is a mental health condition where you use the control of food to cope with feelings and other situations. Anyone can get an eating disorder, but teenagers between 13 and 17 are mostly affected. With treatment, most people can recover from an eating disorder’ (NHS, 2021)
Click here for more information from the NHS explaining eating disorders.
Who could develop an eating disorder? Anyone, of any age, race, culture, gender, or ethnic background,

Types of Eating Disorders – Anorexia Nervosa, Bulimia Nervosa, Diabulimia, Binge Eating Disorder, Avoidant/Restrictive Food Intake Disorder (ARFID), Other Specified Feeding or Eating Disorder (OSFED) / Eating Disorders Not Otherwise Specified (EDNOS), Orthorexia, Rumination Disorder, Pica, Bigorexia.
Causes: Eating disorders are complex. There is no single reason. There can be a range of factors that could combine to make it more likely any one person could develop this condition.
Further explanations: Eating disorders are ever changing and different for everyone. Unhealthy eating behaviours may include but aren’t limited to eating too much or too little or worrying about your weight or body shape.
So many things can be going on at the same time and you can feel like things are so out of control.
You may feel the urge to want to put things in a box or label things you don’t understand, to normalise or minimise what you are experiencing.
Eating Disorders can become a crutch and feel like it is all you have got.
You do not have to focus on recovery if this feels like a long way off. Consider small more manageable steps to help you on the journey of recovery. Small steps are still steps.
Often there are religious holidays, festivals, rituals or periods of our lives that are focused on food. These can be difficult so don’t be afraid to ask for support.
Individual’s experience eating disorders and feelings differently. You could do certain behaviours or experience thoughts and activities that are unhealthy but make you feel good. It can be hard to let that go as that’s a coping mechanism.
Early habits - There can be early signs or habits that are unhealthy for individuals to do. It is a good idea to act quickly. Beat have a 'Know the first signs' poster which you can see to the right or you can download a copy here.
.Back to top/menu
Myths and truths
To view all of the myths please click here.+
- Mental illnesses, especially eating disorders are somewhat more ‘accepted’ now, more 'normal' and common. Still not everyone understands. It is an illness. You’d get treatment for a physical illness, so this is the same
- Individuals may feel alone as eating disorders are so specific and different for everyone. It can feel like others around you have it together and you don’t
- The reality of eating disorders being far from the stereotype. Anyone can have an eating disorder, for any reason. It is not about will power or self-control
- Myth - Eating disorders are about food and body image
Truth - It is often the complete opposite
- Myth - It’s your fault and is your decision
Truth - Cause can be varied. It is complicated. There are a variety of things that effect whether someone goes on to develop an eating disorder
- Myth – You must be a below a certain BMI to get help
Truth - BMI shouldn’t determine if you’re getting treatment or not, that isn’t the only way to measure at eating disorder
- Myth – It is just a phase and will pass
Truth - Don’t wait for yourself to get worse. – early intervention will help you recover
- Myth – I haven’t accessed help before so this will mean I won’t get support because I am not ill enough
Truth - It doesn’t matter if you’re going to your GP or anyone for help for the first time or have a long-term condition, you can get help
- Myth - You’ll have this forever
- Truth - You can recover
- Myth – All eating disorders are anorexia and are all about being skinny.
Truth - There is no standard eating disorder. People of all shapes and sizes can experience an eating disorder
- Myth - You have to be underweight to have an eating disorder. You can see if someone has an eating disorder by looking at them
Truth - Eating disorders are about more than food and weight. You can have an eating disorder at any weight or size. Eating disorders can’t always be seen. What you do see isn’t the whole picture. The issue is much deeper than food
- Myth- Eating disorders are a choice
Truth - Eating disorders are an illness. You can recover. There are so many things that contribute to an eating disorder, like biology/genetics, cultures, trauma
- Myth - Eating disorders only affect young girls
Truth - There is no standard eating disorder. It can happen to anybody of any age, gender identity, culture, and ability. BEAT say that in the UK there are around 1.25 million people who have an eating disorder. 25% of those affected by an eating disorder are male.
- Myth - Something or someone is to blame
Truth - Eating disorders happen for several reasons and are nobody’s fault. There can be lots of contributing factors, trauma, genetics, stress, biology, surroundings, psychology (core reasons)
- Myth - I will be like this forever
Truth - It may be in your life for now, however recovery is possible
.Back to top/menu
Physical health = Mental health
It is a common misconception that eating disorders are about physical looks. Whilst there are physical aspects such as weight loss or gain, bingeing, and vomiting, over or under eating, or over exercising, eating disorders are a mental health illness affecting thoughts and feelings. Physical and mental health are closely linked, and it is important to look after both.
Quiz
Back to top/menu
Signs and symptoms
Anyone can have an eating disorder; you don’t have to experience all symptoms to be struggling with one. Individuals who have their own experiences with eating disorders have put together a list of signs and symptoms to look out for, alongside a list of different eating disorders and their descriptions which you can view here.
.
How to start a conversation
Who to talk to.
When considering who to talk to about any concerns you might have with food, eating, your weight or shape, it is important to find someone you can trust and who can listen to you without judgement. This might be a teacher, a friend, a colleague, or a family member. You might also want to talk to a healthcare professional such as a GP. Choosing a time when you don't feel rushed can be important, and perhaps avoiding mealtimes or other potentially difficult times can be helpful too.
What to say? Helpful phrases and sentence starters+
- ‘I am struggling with…’
- ‘I am finding things hard …’
- ‘I think I need help…’
- ‘I am worried that I am not coping, can I talk to you…’
- ‘Have you got some time for me to talk about something I’m going through…’
- ‘I am not feeling myself at the moment. Can I talk to you?’
- ‘…I’m actually not fine’ – you don’t have too always be ok
You can ask someone to come to an appointment with you.
Helpful things to know:
- People may not understand or react how you’d hope or expect. Try not to let this put you off. Try someone else. Trust someone will listen
- Their reactions are about them and their understanding, it is not about you. It depends on their mental state and capacity at the time but does not mean they will never understand, listen or be there
.Back to top/menu
What might happen if you ask for help?
We know that speaking about this topic with healthcare professionals might seem overwhelming. We want to share some pointers as to what might happen at your appointments.
- Trust yourself at the GP surgery. You can have a say in your appointment. If your GP suggests you’re fine and you know you are not, don’t take no for an answer, you can ask at the reception to see another doctor/a doctor that is good with mental health. It is also ok to take someone with you to support you. You can also write down specific points you want to say
- Professionals will want to check your health. They need to get a clear understanding about your physical wellbeing to view you in a holistic way (all aspects of your whole self). Some may take blood tests, ECG’s, (recording of your heart activity) blood pressure, and weigh you. You can ask for this to not be shared with you if you choose, and you don’t have to look while they do these tests
- You may be referred to other services and specialists, and you may go on waiting lists. This may mean you could come across different professionals and specialists in your journey such as counsellors or therapists, specialist eating disorder staff, mental health staff, social workers, health care assistants, nurses or psychologists/psychiatrists
- Try not to be put off by professionals if they do not understand or if your experience isn’t as positive as you had hoped. Sometimes the advice you get might not always work for you. Professionals do not always get it right first time. Please don’t let any of this put you off asking for other support
.Back to top/menu
Wellbeing tool kit
 Self-care
Self-care
- Breaking the cycle, if may be helpful to look at the cycle of change - Beat has helpful information on this that can be viewed here
- Look after your physical health. If you are physically unwell don’t avoid seeing a health care professional
- Basic self-care, like brushing your teeth or having a shower is important for your physical and mental health in helping you feel better. Try to set yourself small goals, like getting dressed and washing your face or accepting that you’re allowed to look after yourself
- Prioritise yourself, this includes giving yourself time to rest and sleep, self-acceptance and self-love
Healthy distractions
- Puzzles, games, reading a book, listening to some music, meditation, taking a bath, yoga, Pilates, tai-chi
- Put your favourite film, TV program or music on
- If your ways of coping include self-harming or inflicting pain on yourself, try less damaging alternatives such as pinging an elastic bands, writing on your skin or holding ice cubes. These physical distractions could help
- Volunteer/charity work – this can be a great way to boost your confidence and aid your recovery
 Connecting - Is there someone you can talk to?
Connecting - Is there someone you can talk to?
- Have a catch up with a friend or family member. Contact someone you trust, it doesn’t have to be a phone call, and you can talk about anything
- Beat have a helpfinder on their website to help you find support in your area
- Beat has helplines you can call which are open 365 days a year from 9am–8pm during the week, and 4pm–8pm on weekends and bank holidays and they also have online chatrooms, one-to-one online advice chat options, 'Blossom' - which is an online structured group to help support those who are managing their eating disorder whilst waiting for NHS treatment and 'Invicta' - which is an online unstructured chat group where others with similar experiences can share helpful advice for recovery and their experiences, the chat room is moderated by BEAT employees so posts are approved before being 'published' to the group to ensure no posts are triggering or inappropriate
 Mindful- Find what works for you — gratitude, appreciating the little things
Mindful- Find what works for you — gratitude, appreciating the little things
- Try to step back and reflect on what is going on for you right now. You might find it helpful to write this down
- Get some fresh air. Take in your surroundings—connect with nature
- Writing down things to look forward to, reasons to recover
 Get creative — journal, scrapbook, write down your reasons to recover, paint, draw, crochet, or knit
Get creative — journal, scrapbook, write down your reasons to recover, paint, draw, crochet, or knit
- Write down your own positive affirmations and gratitude. You can do this on post-it notes, in a journal or on your phone
- Doing things that make you happy
Use recommended sites like NHS, Mind, BEAT, PEDS. Information can be damaging and unhealthy. Being aware of unhealthy sites that encourage negative behaviours/thoughts/actions. There can be negative and positive information online.
.Back to top/menu
Pandemic
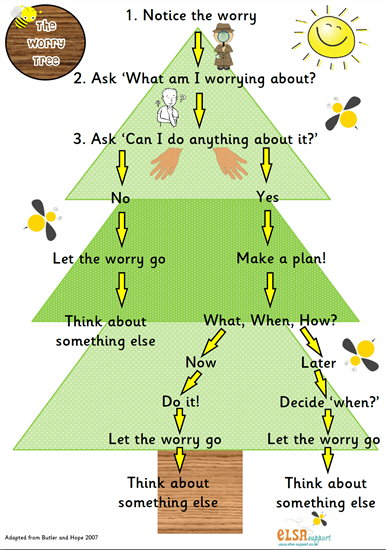 Coping with the change during the pandemic. It is a worrying time at the moment for many people, so anxieties are bound to be heightened, try and take things one step at a time (BEAT has information about shopping, routines and anxiety during the pandemic). You can write a worry list or worry tree here.
Coping with the change during the pandemic. It is a worrying time at the moment for many people, so anxieties are bound to be heightened, try and take things one step at a time (BEAT has information about shopping, routines and anxiety during the pandemic). You can write a worry list or worry tree here.
Beat has a section on their website with information on how to cope during the pandemic which you can view here.
- Being eligible for a vaccine. For information on vaccinations please click here
- Not wanting to get help with your physical and/or mental health challenges because of the effect the pandemic has had. Your wellbeing is important so you should still seek help, click here to go to view resources available to support you
- You might not initially see a medical professional face to face due to the pandemic, however you might get a phone or video call. This may change depending on the restrictions in place at the time you make contact
- Worrying about life post pandemic and social interactions can be triggering. Try not to rush yourself, trust how you are feeling and be kind to yourself when you are entering a difficult situation. Perhaps you could speak to a friend about your worries to set some goals for yourself. Try not to feel that as lockdown is easing you have to say yes to making plans or going out, you can say no if you don’t feel ready. You can make plans within the limits that you feel comfortable with
- Routines and rules changing can be disturbing. Setting yourself a healthy routine to provide some structure to your time can be useful
- You may be concerned about shopping. It could help you to make a shopping list for the items you need or want to buy. You can go shopping at quieter times in the day depending on opening hours (between 7am-9am and 7pm-9pm)
- Campaigns, advice and social media messages can be overwhelming. Advice and information from the government and other organisations are blanket messages that do not cover individual aspects of health. They aren’t always relevant to everyone and often can miss important aspects. Take a break from the news, you don’t have to engage with everything all the time
- Whether there is a pandemic or not you are worthy of help and there is support. It just might look different
- The pandemic will not last forever
- Pressure of being encouraged to exercise, socialise and ‘be happy’ because everything is returning to normal. This can be hard to manage and work through so be kind to yourself and focus on your mental wellbeing
.Back to top/menu
Support information
There is appropriate support and help for what you are going through.
Things you can do to make it easier for you when/with getting help:
- Ask someone to come to an appointment with you
- Making notes/plan of what you want to say
- Plan something nice after your appointment
- Choose a time and a place you are comfortable with
- Take it slow – you do not have to say it all in one appointment. Remember it is the start of a conversation and what’s important is getting it out in the open
What to do if you are unhappy with the service you access/can’t access:
- Firstly, you could speak to the service themselves through their complaints process. Don’t worry, this won’t prevent you from accessing further services if you require them
- If you wish not to speak to the service yourself, you are welcome to contact The SUN Network or you could go to Patient Advice and Liaison Service (PALS)
- There are a variety of other support services out there so if the one you are currently with isn’t working for you don’t worry
While you wait:
You could have been: referred and are on a waiting list, moving out of/into areas, moving back to home after being away, moving into community, inpatient or outpatient services or you could be between children and adult services and waiting to get support.
- Monitored chat rooms – Beat has helplines you can call which are open 365 days a year from 9am–8pm during the week, and 4pm–8pm on weekends and bank holidays and they also have online chatrooms, one-to-one online advice chat options, 'Blossom' - which is an online structured group to help support those who are managing their eating disorder whilst waiting for NHS treatment and 'Invicta' - which is an online unstructured chat group where others with similar experiences can share helpful advice for recovery and their experiences, the chat room is moderated by BEAT employees so posts are approved before being 'published' to the group to ensure no posts are triggering or inappropriate
- Self-care
- You can speak to your GP. They can help in different ways, they may offer to sign you off work
- Occupational support may be offered
- There are private healthcare avenues available
- You could access other local voluntary sector organisations
- There are helplines available to call
.Back to top/menu
Services (what is on offer)
- Support groups - PEDS and BEAT have support groups. These can be accessed through self-referrals, GP referrals and online portals. Due to the limited amount of support groups available, they can be at times difficult to access. There are however other support services you can go to and other resources you may find useful
- Support services - Keep Your Head has a list of support services for mental health and wellbeing
- The SUN Network co-produced some information leaflets, with the help of carers of loved ones with eating disorders and individuals who had lived experience of an eating disorder. The two free information leaflets can be accessed via this link and a leaflet about medical monitoring with eating disorders can be read and download here
- School/college/uni
- NHS - Cambridgeshire and Peterborough Foundation Trust (CPFT) Eating disorder services. CPFT run the Eating Disorder Service locally. Most people will be seen as outpatients, with a small number requiring a hospital inpatient stay. To access support for an eating disorder, please visit your GP.
- CPFT's Keeping Safe Programme - The Keeping Safe programme is the first step in your treatment. It has been developed to provide information to help you begin to make sense of your difficulties and to encourage you to take steps to minimise any potentially harmful effects caused by your eating disorder whilst you are waiting for treatment. The aims of the Keeping Safe programme are:
- to provide information about eating disorders
- to promote a better understanding of the effects of eating disorders
- to give guidance and harm minimization tips to help you keep yourself safe whilst you are waiting for treatment
- Primary Care Mental Health Service (PCMHS) - is a service that covers all surgeries in Cambridgeshire and Peterborough. The service provides specialist mental health support for GP surgeries so that patients with mental ill health can access prompt advice and support, receive help in a community setting and experience a more joined-up approach to care.
- Your GP surgery
- Beat have a helpfinder on their website to help you find support in your area
Voluntary organisations:
 Personalised Eating Disorder Support - PEDS - (Self-Refer) - offers assessment and support with signposting and where appropriate to service users, families and loved ones and professionals. We offer our service users individual sessions which are tailored to meet the unique needs of each person. We also provide family sessions which include practical help, education and support. We operate mostly remotely and sessions are via Microsoft Teams or Zoom. This includes assessments, 1:1s and groups (service users and carers). Face-to-face sessions, if required, are held at Boroughbury Medical Centre
Personalised Eating Disorder Support - PEDS - (Self-Refer) - offers assessment and support with signposting and where appropriate to service users, families and loved ones and professionals. We offer our service users individual sessions which are tailored to meet the unique needs of each person. We also provide family sessions which include practical help, education and support. We operate mostly remotely and sessions are via Microsoft Teams or Zoom. This includes assessments, 1:1s and groups (service users and carers). Face-to-face sessions, if required, are held at Boroughbury Medical Centre CPSL MIND is a mental health charity which promotes positive wellbeing across our communities and supports people on their road to recovery from a wide range of mental health challenges. They offer online support, community initiatives to connect people, counselling, Cognitive Behavioural Therapy, peer support groups, Perinatal services and opportunities to get involved with training, volunteering, campaigning and fundraising
CPSL MIND is a mental health charity which promotes positive wellbeing across our communities and supports people on their road to recovery from a wide range of mental health challenges. They offer online support, community initiatives to connect people, counselling, Cognitive Behavioural Therapy, peer support groups, Perinatal services and opportunities to get involved with training, volunteering, campaigning and fundraising Centre 33 — exists to help every young person in Cambridgeshire fulfil their potential and overcome problems through a range of free and confidential services - including housing, sexual health, family problems, and bullying
Centre 33 — exists to help every young person in Cambridgeshire fulfil their potential and overcome problems through a range of free and confidential services - including housing, sexual health, family problems, and bullying Lifecraft is a user-led organisation for adults in Cambridgeshire and Peterborough who experience mental health difficulties. They offer a range of free mental health services to help and support individuals in their wellbeing and recovery
Lifecraft is a user-led organisation for adults in Cambridgeshire and Peterborough who experience mental health difficulties. They offer a range of free mental health services to help and support individuals in their wellbeing and recovery Illuminate is an organisation specialising in mental health coaching and training to help make positive changes
Illuminate is an organisation specialising in mental health coaching and training to help make positive changes Beat – Beat provides Helplines for people of all ages, offering support and information about eating disorders no matter where you are in your journey. These Helplines are free to call from all phones.
Beat – Beat provides Helplines for people of all ages, offering support and information about eating disorders no matter where you are in your journey. These Helplines are free to call from all phones.
Our Helplines are open 365 days a year from 1pm – 9pm during the week, and 5pm–9pm on weekends and bank holidays. Support on the Helpline is available by phone, email, webchat (live link) through our social media accounts and by letter. Calls to the helpline are free from landlines and mobile phones within the UK and do not appear on itemised bills.
Sometimes our lines are busy. If you can't get through immediately, please do try again or try our one-to-one web chat or send us an email.
If you are in need of urgent help or medical advice for yourself or someone else, please contact 999 or the Samaritans on 116 123 if you or someone else is in immediate danger. If you are looking for medical advice, contact your GP or 111.
Helpline for England: 0808 801 0677
Helpline for Scotland: 0808 801 0432
Helpline for Wales: 0808 801 0433
Helpline for Northern Ireland: 08088 010 434
 SEED – (Support and Empathy for people with Eating Disorders) are a voluntary organisation and registered charity whom have first-hand experience of eating disorders and make a different to others who are challenged with this illness
SEED – (Support and Empathy for people with Eating Disorders) are a voluntary organisation and registered charity whom have first-hand experience of eating disorders and make a different to others who are challenged with this illness
.Back to top/menu
Resources
Books: Authors of lived experience and carer books:
- Hope Virgo
- Emma scrivener
- Jenny Langley
- Tina McGuff
- The Invisible Man - A Self-help Guide for Men With Eating Disorders, Compulsive Exercise and Bigorexia
- Samuel Pollen - author of The Year I Didn’t Eat
- Christopher Eccleston - I Love the Bones of You
- Rhik Samadder - I Never Said I Loved You
- Andrew Walen - Man Up to Eating Disorders
- MaleVoiced - this website is specifically for male ED suffers and has some brilliant resources including this great list of books
- Beat have suggested books
- Mindful Eating: A guide to rediscovering a healthy and joyful relationship with food - By Jan Chozen Bays
- Life without ED by Jenni Schaefer
- 8 keys to recovery by Geneen Roth
- The Inside Scoop on eating disorder recovery: Advice from two therapists who have been there by Colleen Reichmann and Jennifer Rollin
- Goodbye ED, Hello Me: Recover from your eating disorder and fall in love with life by Jenni Schaefer
- Body Image Workbook
- The secret language of eating disorders, Peggy Claude-Pierre
- The War of art - Steven Pressfield
- Sick enough: A guide to the medical complications of eating disorders by Jennifer L Gaudiani
-
Thinsanity by Glen Mackintosh
- Janet Treasure books - aimed at carers
Podcasts:
Apps:
Websites:

There are resources for carers which can be viewed here.
.
Helplines:
- Lifeline - 11am-11pm every day 0808 808 2121
- NHS First Response Service. In a mental health crisis? Call NHS 111 option 2
- Samaritans - 24hours a day, 365 days a year. Free line 116 123
- Beat (Adults) - Call for eating disorder support - 0808 801 0677
- Beat (Student Line) - 0808 801 0811
- Beat (Under 18's) - 0808 801 0711
- SEED Advice Line - (01482) 718130
- National Centre for Eating Disorders - 0845 838 2040
- Your GP surgery
Caring for someone with an eating disorder
 Welcome
Welcome
Do you provide care or support for a loved one, friend or colleague with an eating disorder?
Here are warm words and ideas from parent/carers to help you support someone with eating challenges.
You are not alone.
The information on this page has been collected from discussions at carer support groups. The summaries of these conversations are linked throughout the page and also in our resources section under books.
Note - This guidance relates to adults. Many of the ideas are relevant to children and young people, too, but parents should always ask the person who is treating their child how best to help.’
Signs and symptoms
Anyone can have an eating disorder; you don’t have to experience all symptoms to be struggling with one. Individuals who have their own experiences with eating disorders have put together a list of signs and symptoms to look out for, alongside a list of different eating disorders and their descriptions which you can view here.
Early habits - There can be early signs or habits that are unhealthy for individuals to do. It is a good idea to act quickly. Beat have a 'Know the first signs' poster which you can see the the right or you can download a copy here.
Questions you may be asking yourself:
We are worried that our loved one might have an eating disorder – what should we do? +
Scenario
There are a wide range of symptoms and signs of an eating disorder, you may have noticed a few of these when with your loved one. Eating disorders are a serious illness and it is important to catch them early on before they can develop further; recovery is possible and more likely the earlier an eating disorder is identified and treated.
What can we do to help?
- Start up a conversation about what you’ve noticed and express that you’re concerned for your loved one’s health and wellbeing
- Use open questions to help your loved one understand how they are feeling and why they may be doing certain behaviours
- Your loved one may get defensive and not wish to speak about how they’re feeling and acting, be patient and ask the big questions in a low stress moment
- Ask your loved on if they would be willing to talk to someone about how they are feeling and inform them on how serious eating disorders are
- You can encourage your loved one to speak to their GP, another health professional or support service
Anything Else?
Find out about eating disorders. Beat are the eating disorder charity for the UK. NHS also have information on their websites about eating disorders.
More Ideas
See pages 11 and 12 of Skills-based Caring for a Loved One with an Eating Disorder by Janet Treasure, Grainne Smith and Anna Crane. Routledge. ISBN 978-1-138-82663-2. 2
Carers support group summary
What is the best way of caring for our loved one? +
Scenario
On the face of it this may seem a strange question but anyone with lived experience will tell you how counter-intuitive caring for a loved one with an eating disorder is. For example, for many sufferers, especially in the early days, their eating disorder gives them something positive, i.e. a way of coping with unbearably strong emotions, thoughts and feelings. We see eating more healthily as a way of getting better but they see taking away their eating disorder as a threat and something to be resisted. One carer described it as a ‘topsy turvy world’ where ‘you will almost certainly have to learn some new skills’.
What can we do to help?
At a support group meeting, two former sufferers talked about their recovery journey, the important role their families played and how best we as parent/carers can help:
- Unconditional love - being there and listening; being non-judgemental
- Showing that you care - one described how her mother put notes under her bedroom door at times when discussing her illness more openly was difficult, which demonstrated that she was not blind to her struggle
- Connecting - about non-eating disorder subjects / activities, so that the illness does not define the entire relationship
- 'Nudging' - making an appointment for her and telling her about it but leaving it up to her as to whether she attended or not
'Be more dolphin' in her book (see below) Janet Treasure uses animal metaphors to describe our behavioural and emotional responses. The dolphin, who nudges our loved one’s head above the water but lets them do the work of getting safely to shore, is contrasted with the rhino, who charges in with the answer and makes our loved one back into a corner. The kangaroo, who puts their loved one in their pouch to protect them – a perfectly natural parent/carer reaction – is also unhelpful because our loved one never has to face up to getting better. These metaphors are really helpful.
Anything else?
- Remember the ‘3 Cs’ - stay Calm, be Compassionate, show you Care
- Sometimes you will need to step back before you step in again – count to ten and say the third thing that comes into your head, not the first
More ideas
- See Chapter 5 of ‘Skills-based Caring for a Loved One with an Eating Disorder’ by Janet Treasure, Grainne Smith and Anna Crane. Routledge. ISBN 978-1-138-82663-2. 2nd Edition
- See the videos signposted in the Carers Support Leaflet
What should we do if our loved one becomes overwhelmed / distressed? +
Scenario
There are many occasions when our loved one might become extremely upset. Not surprisingly, mealtimes can be a flash point. Shouting, screaming, hitting themselves, throwing food – sometimes this happens. Something could trigger your loved one to react in a distressed or overwhelmed way, this could be shopping, a social occasion. Anxieties can build up over a varying length of time.
What can we do to help?
- In advance of a situation, encourage our loved one to a use a calming strategy e.g. meditation, taking the dog for a walk
- During a situation there are other strategies to help that can be applied, e.g. breathing techniques or agree a distraction, such as watching the television
- Validate and empathise so that they know they are not making it up and that you recognise how difficult it is
- Advanced planning and discussions at a calm time prior to events or situations, about what your loved one may find helpful
Anything else?
- Stay calm, don’t get drawn into the fight
- Step back if necessary, step in later when you feel up to it
- Look after yourself
More ideas
See pages 188-191 of ‘Skills-based Caring for a Loved One with an Eating Disorder’ by Janet Treasure, Grainne Smith and Anna Crane. Routledge. ISBN 978-1-138-82663-2. 2nd Edition.
Carers support group summary, 26th May 2020, page no: 24 and 6th October 2021, page no: 9.
Our loved one keeps asking for reassurance – what should we say? +
Scenario
Most carers will have experienced their loved one seeking reassurance by constantly asking the same question. ‘Do I look fat?’ ‘Do these clothes fit alright?’ ‘Does it matter if I go out for a run?’ It is understandable that we want to reassure our loved one that they are not fat, that their clothes do fit and that it doesn’t matter if they go out for a run. However, although this relieves their (and our) immediate anxiety it does not help in the long run; they will simply come back to us and keep asking. This is what is called ‘the reassurance trap’.
What can we do to help?
- Discuss the ‘reassurance trap’ in a low stress moment. Listen to their concerns and help them ‘name their feelings’. Talk about how their anxiety will pass and won’t be so much of a problem next time. Agree what you are going to say the next time they ask you a particular question
- Respond with empathy, warmth and, if appropriate, your agreed response: ‘‘I can see you are really anxious, as we discussed it’s not helpful for me to answer this question’. ‘I know you are really anxious, I know you can make the decision about this’. ‘I understand you are worried, you know the answer to that question’
- Be consistent, don’t ‘give in’. You may need to be like a stuck record (remember those?), playing the same line again and again
Anything else?
- Stay calm. Your loved one may become very distressed – it will pass
- Praise occasions when your loved one successfully manages to cope with their anxiety
More ideas
You can read more about ‘Reassurance Seeking’ here.
What should we do if we get overwhelmed/distressed? +
Scenario
Looking after a loved one who is unwell or going through an emotionally and physically demanding illness may take a toll on your wellbeing. You may experience challenging times, barriers or inconveniences that cause you to become overwhelmed and/or distressed. It could be a very draining time that you are going through and it is natural to feel sometimes exhausted from everything.
What can we do to help?
- Self-Care
- You may want to seek professional help for yourself
- Be open and honest with your loved one about needing support from the people around you. It is important to respect their confidentiality. Equally they need to understand what you are going through and what will help you
Anything else?
Setting boundaries is also important – please see the next question for more information on setting boundaries.
You are human and are likely to experience your own challenges. Remind yourself that it is ok to have rest days.
More ideas
You can view different support services for yourself here.
Carers support group summary, 1st September 2020, page no: 75, 3rd November, page no: 34 and 9th February 2021, page no: 121.
How do we prevent our loved one’s eating disorder taking over our lives? +
Scenario
When living with a loved one with an eating disorder it is easy to slip into the role when you will do anything to help your loved one. Acting like this is accommodating the illness and does not help in the long term.
You can spend a lot of time (and money) around food; planning, shopping, preparing, cooking and eating.
- Buying the right ingredients – e.g. a particular brand of bread with the lowest calories even if that means visiting several shops to find it
- Prepping in a very specific way, with arguments about how food should be prepared, if there is enough/too much. Then the demands about how, where and when the meal is eaten and with whom
What can we do to help?
Know and set boundaries:
- These are ground rules unique to your family, and can be difficult to enforce if clear rules not agreed upon and backed up by all family members, e.g. Agree to a shopping list and if that brand is not available buy an alternative and calmly explain why you can’t go to several shops (have to get to work, need time for hobby/dog walk).
- Model keeping family life as normal as possible
Family problem solving
- Talk to individuals before bringing everyone together, pay particular attention to any siblings
- When everyone is calm, make a list of things that are expected (from everyone), and things that are unacceptable to refer to for confidence and consistency when challenged
- Make this a set of family ‘House Rules’ (rather than eating disorder-specific boundaries)
Try to hold the important boundaries, the lines you will not cross.
- But roll with it if it is not working, try again at a calmer moment, be prepared to re-negotiate
Anything else?
Stay calm.
Look after yourself by regularly setting aside time to spend with your partner/friends/relations when you don’t discuss the eating disorder.
Focus on the individual, not their illness.
Show unconditional love.
We are only human, so we need to allow ourselves to have time for us.
More ideas
Beat website
FEAST website
Information on why boundaries are important in eating disorder recovery
Skills based caring for a loved one with an eating disorder. Page 105-106 and 205. - Skills-based Caring for a Loved One with an Eating Disorder by Janet Treasure, Grainne Smith and Anna Crane. Routledge. ISBN 978-1-138-82663-2. 2nd Edition.
Information and skills for when you may be falling into eating disorder traps, for example portion sizes, safe foods, activity/exercise, pretending you didn't see something and shopping for the eating disorder.
Carers support group summary
How can we keep going – we’re feeling done for and this illness goes on for such a long time? +
Scenario
It can take a long time to recover from an eating disorder and there are many ups and downs along the way. As a carer this is emotionally and physically exhausting. All you want is for your loved one to be better, but the finish line seems nowhere in sight. How do you keep going?
What can we do to help?
- Maintain your hobbies and interests that are nothing to do with the eating disorder, so that they become a sanctuary where you can recharge your batteries
- You might find using a notepad to write everything down to be helpful as it can be used to get thoughts and feelings out of your system
- Stay in touch with a small number of trusted friends
- Sometimes it is important to stop, step back and pause before you step in again
Anything else?
- Remember to tell yourself that recovery is the most likely outcome
- Keep active. A walk will improve your mood. Proof? Note how you feel before you go and when you get back
More ideas
Watch the ‘Carer Fatigue’ video here.
Where can I get support for myself? +
Scenario
The constant pressures involved with living with and supporting a loved one with an eating disorder can be overwhelming. It can take over your life leaving you exhausted, pressured and hopeless. It may be difficult to share what you are going through with others, so you could feel alone.
What can we do to help?
- Look after yourself. Be prepared to seek professional help yourself
- Be open to connecting with people who have similar experiences. Support groups can be invaluable. Share the burden with others
Anything else?
More ideas
How can we talk with / respond to our loved one about topics or questions that might provoke an angry or negative response? +
Scenario
There are many occasions when what we think is the most sensible thing to do is not what our loved one wants to hear and/or they ask us a question and we know they will not like our answer. They may become angry or upset and the outcome is unlikely to be positive. Arguing doesn’t work, our loved one will come up with more ideas for why they are right, and you are wrong, making the problem worse.
What can we do to help?
- Be curious rather than judgemental. For example, if our loved one is threatening to discharge themselves from hospital against advice, ask ‘How are you going to manage at home?’ rather than saying ‘I don’t think that’s a good idea’
- Refer to the higher authority. ‘Your doctors have agreed what’s best for your treatment, we’re here to support you with that’. The ‘higher authority’ can be something you’ve read or something that you’ve heard
- Pick a calm moment - if emotions are high, it is unlikely that any discussion will be productive
- If your loved one keeps asking the same question, answering might help them in the short term but not in the long term. Plan what you are going to say in advance e.g., ‘We agreed I wouldn’t answer that question again because we have discussed it before’. ‘I understand you are worried; you know the answer to that question’
Anything else?
- Difficult conversations need lashings of empathy, e.g. 'I see that this is really hard for you to talk about, and I am so pleased that we are having this conversation. How best can I help?'
- Remember the ‘3 Cs’ - stay Calm, be Compassionate, show you Care
- Ask yourself, ‘What would a good Dolphin do?’ In other words, don’t charge in with the answer, like a Rhino, or avoid the question, like an Ostrich… Do use open questions to encourage your loved one to find their own answers
More ideas
Although more targeted at children and young people than adults, this link has some very relevant advice about non-combative communication styles.
What do I need to know about consent and confidentiality? +
Note - Confidentiality is very important. Confidential information about a patient should only be shared with their explicit consent. Confidential information about, or provided by us as parent/carers should only be shared with our explicit consent.
This guidance relates to adults.
Scenario
At the beginning of any treatment, whether at the GPs, with a Community Team or in a specialist inpatient unit, our loved ones will be asked if they give consent to share information with us. Quite often they do not, or give consent for only some information to be shared, or only with some people. This can make us feel as if we are providing support ‘in the dark’. It can also make us feel side lined, despite the efforts we are making, and this can lead to resentment. How do we deal with this?
What can we do to help?
- Be reassured - confidentiality should and will be breached if your loved one’s life, or someone else’s life, is at risk
- In the absence of consent staff are encouraged to share non-confidential information with parents/carers because the more we know and understand about our loved one's illness and treatment the better we can support – ask if this doesn’t happen
- If you have information that is important to your loved one’s recovery you can always pass it on in confidence - you might not get a response, but it will be taken into consideration; the team supporting your loved one’s recovery would rather know than not
Anything else?
- Try to plan. In the depths of the illness, or the heat of an emergency admission, your loved one’s response may be different to their view in healthier, calmer moments
- Asking permission can be very helpful: ‘What would you want me to do if....?’ Your loved one may be willing to write this down so that the professionals do not have to take your word for it
- Consent should be regularly reviewed by the professionals – you can ask if this is happening
More ideas
- All service providers will have a Consent and Confidentiality Policy. You could ask to see this if you had concerns
- Cambridgeshire and Peterborough NHS Foundation Trust has produced a ‘Common Sense Confidentiality’ leaflet that explains clearly what should happen and what you should do if you have concerns
Long distance caring - How can we help our loved one if they live away from us? +
Scenario
Often our loved ones may not live with us; they may be moving in with a friend, a partner or relative, they may be at university or have a new job and move away. It can be a worry as not being able to physically see a loved one can leave you wondering how they are (as when they are close, spotting signs are easier). It also can be challenging if they do not talk to you about their eating disorder.
What can we do to help?
- They are adults; this is their chance to test out real life managing an eating disorder. Give them support and have belief in them and offer unconditional support. ‘I think you’re really brave getting this job and moving away, if you need us we are here for you’
- Check in with them by text, phone or video call; ask open questions ‘How has your week been?’ ‘How are you feeling?’ They can choose how they respond and sometimes a text or quick call talking about something other than the eating disorder can open channels for more conversations
- Ask permission to ask questions, ‘Would you mind if I ask you a question about your eating disorder?’ ‘Can I ask you about how you are getting on with your meal plan? Its ok if you don’t want to discuss it with me.’ Giving them choice to answer
Anything else?
- Often you can get a feel for how someone is doing by a quick message; ‘I’m wondering if you are struggling a bit, you seemed a bit anxious on our call, I’m here if you need to chat?’ This can keep the channels of communication open
More ideas
Motivational interviewing techniques can be helpful. E.g., when you are talking on the phone ask lots of open questions, check that you’ve understood what they are saying (that will help them to sort out their own thoughts, too), listen, listen, listen, pull it all together and don’t give an opinion unless asked.
What can we do about partners / friends / family who react differently to our loved one’s illness? +
Scenario
This is very common and very complex. If one partner has had the lead caring role, the other may feel left out, or begrudge receiving less attention. Friends may not understand why you don’t just tell your loved one to snap out of it and eat properly. Family may say unhelpful things unwittingly, e.g. ‘You’ve put on weight, You’re looking so much better’.
What can we do to help?
- The best thing you can do is share and spread the load. Be open and honest about the situation and the illness, and how it is affecting you as a family. Include your loved one in this decision
- Make sure that you prioritise time for the relationship, whether it is with your partner / a parent / a special friend. Relationships need nurturing
- Make a real effort to talk as a family. If you don’t help them they will probably say the wrong thing
- If you have been the main carer, be generous and supportive if your partner, or a friend, wants to be more involved. This can feel a bit threatening - 'Am I not good enough?' - but it could be really helpful, to you and them
Anything else?
- Remember that recovery is not only possible, it is the most likely outcome. It will not be like this for ever
- Don't feel guilty. Relationships sometimes fail even in that 'normal' world outside of the strange world we inhabit
More ideas
See ‘Eating disorders: a guide for friends and family’ on the BEAT website.
Carers support group summary, 23rd March 2021, page no: 141.
How can we best support our loved one’s siblings? +
Scenario
When you have a loved one who is struggling with a serious mental illness, a lot of focus can be around them and what they need. For your loved one’s siblings it can be shocking to see their sibling’s health decline and to learn of how they have been struggling. Our loved ones siblings may need some support too.
What can we do to help?
- Reassure them that they have not done anything to contribute to their illness, it’s understandable to feel overwhelmed and they don’t need to feel guilty about getting on with their life and enjoying themselves. In fact by doing this they are actually showing what ‘normal’ is and are being a good role model for their sibling
- Check in with your loved one’s siblings on how they are feeling. Give time and space for them to ask questions
- Keep lines of communication open about ‘normal life’. Don’t let the eating disorder be the focus of every conversation, enjoy some things that are nothing to do with the eating disorder
Anything else?
- Beat have an online video based peer support group called Solace, which is hosted over zoom, and it is for anyone who is supporting someone with an eating disorder
- Support them to help and contribute as much as they feel able without pushing them
More Ideas
Carers support group summary, 18th August 2020, page no: 65 and 9th March 2021, page no: 137.
Our loved one is stuck- how can we help motivate them to make the next step in their recovery? +
Scenario
Throughout your loved ones eating disorder there may be times that they become stuck and may find it hard to make changes. They may be in an action phase where they are trying to introduce new foods and are unable to make that change; they may be attempting to go out for a coffee and introducing a snack as well and feel overwhelmed; they may be stuck in a binge purge cycle or they may be over exercising unable to decrease their activity.
It can feel challenging as someone attempts to make changes and becomes stuck, provoking a range of emotions in our loved ones such as fear, anxiety, failure, frustration, and also in you as a carer.
What can we do to help?
- Understand how big a challenge making changes can be to someone. Empathise and acknowledge how hard it can be to make that change. It may take a few attempts before change happens, your loved one may feel disappointed with themselves and feel like they are letting you down too
- Active listening- use open questions; ‘How are you feeling about going for a coffee?’ Reflect what they have said to you, to show you have listened and try not to offer advice
- Give feedback – ‘I can see you are thinking about trying to add a snack in, that’s great that you are thinking about trying, I can see it’s making you anxious.’ ‘I thought that was really brave you going out for a coffee with your friend.‘
- Allowing our loved to come to their own conclusions about a decision, ‘On the one hand you really want to stop running every day because the doctor has said you are at a really low weight, and I understand it’s not that easy to just stop. I wonder if you have any ideas on how to work on that?'
- Try and recognise the emotions that are generated by being stuck and trying to implement change. Offer words of support and encouragement ‘I can see it’s causing you some anxiety that you haven’t done any exercise today. That’s not a great feeling, would you like to watch a film or play a game?
- Motivation- a life to get well for. Model living your life, invite them to join activities that you both enjoy. Focus on the positives in their life; ‘Your day volunteering is really tiring, and your body needs energy to do that, have you any ideas to help you?’
Anything else?
Small steps are key to making changes, maybe just going to a coffee shop and sitting there, and even if your loved one couldn’t achieve their plan, acknowledge that you thought they did well to join you and reiterate you will support them to try again when they are ready. Being patient and accepting that being stuck is a hard place to be, for both them and you.
More ideas
Motivational interviewing, see pages 94-99 of Skills-based Caring for a Loved One with an Eating Disorder by Janet Treasure, Grainne Smith and Anna Crane. Routledge. ISBN 978-1-138-82663-2. 2nd edition.
You can watch a video about the stages of change here.
Our Loved one is being discharged from a specialist inpatient unit- how should we prepare for this and what should we do? +
Scenario
An inpatient admission stay can vary in length of time. Before discharge your loved one will be invited to a Care Plan Assessment (CPA) with all the professionals involved in their care to discuss how their treatment will be continued. Attending the CPA (with consent) will be helpful to support your loved one on the next stage of their journey. An inpatient stay will have involved lots of support around mealtimes, snacks, and many other areas of the eating disorder; it will have been very structured and your loved one may feel anxious or apprehensive at having to continue their recovery at home. It may be that your loved one struggles to stick to their meal/ snack plan and that causes them some distress. It also may be an anxious time for you.
What can we do to help?
- Offer to make a plan together; how would your loved one like to be supported by the family? What might be helpful/ unhelpful? Do this at a mutually agreed time, away from mealtimes
- If they struggle to stick to their meal plan - acknowledge that following it may be difficult, praise their efforts with how hard they have worked to get this far, empathise how challenging it is to do this themselves and offer your support, 'How can we help you around mealtimes?'
- Try not to show your anxiety or disappointment around missed snacks or meals. Empathise, try and offer a non- judgemental response. 'I understand this might be difficult to eat your snack and you’re disappointed you couldn’t eat it, I wonder if there is a way I can help you next time?'
- Refer to the medical professionals if you have concerns, they may not be able to share any information but you can tell them if you notice any worrying signs of the illness
Anything else?
Don’t be surprised to find there may be ups and downs in recovery. Your loved one’s recovery may not follow a linear path after their inpatient stay and they may still have work to do, this can create anxiety for them and you.
Try and focus on activities that you can do together that aren’t based around food. What are their interests?
Model living a normal life. Go to the cinema, have days out, invite them and also allow yourself time off too, supporting someone in their recovery can be challenging.
More ideas
Be open to connecting with people who have similar experiences. Support groups can be an invaluable. Share the burden with others.
BEAT have a range of support services available - helplines, peer-support, echo - BEAT's peer support network and on online chat service. Services for Carers (beateatingdisorders.org.uk)
Our loved one is self-harming as well as not eating – what can we do? +
Scenario
An aspect of an eating disorder could be causing other physical harm to themselves as a way of coping. Self-harming can often be a way of feeling something at a time when someone is feeling nothing or is experiencing negative thoughts.
What can we do to help?
- You can look out for warning signs, tissues, scarring or wounds, or broken razors/sharpeners, hiding arms or legs more than usual. You could suggest less harmful ways of relieving pain like elastic band twanging or holding ice cubes
- Look into stress relief toys for adults
- Try to stay Calm, be Caring and show Compassion. Recognise some triggers for your loved one and empathise with them to help them express their feelings. You can approach their self-harming in a way that is caring by saying ‘That burn looks like it might need dressing’ or ‘Your cut may need some care’ as they can then decide what to do
Anything else?
Be curious for the reasons your loved one is doing this behaviour, think about what purpose it serves. They may be trying to say something but can’t express it which is something we can help with.
More ideas
How do our loved ones co-occurring mental health conditions affect their treatment and the support we should give? +
Scenario
Alongside an eating disorder your loved one may be suffering from other mental health disorders such as Anxiety, Depression, OCD, Self-harm, Substance or Alcohol abuse. These may have been present before the eating disorder began or may have developed as a result of the eating disorder.
Your loved one may be experiencing acute anxiety when they are faced with making changes, which may also extend out into their wider life such as school or work. The physiological changes of an eating disorder may also impact on your loved ones mental health. Self- harm may be a coping strategy to manage their distress. For more information on this click here. All of these things are incredibly hard to watch someone you love go through.
What can we do to help?
- The three Cs- Caring, Calm and Compassion. Acknowledge their struggle, empathise with how they feel and stay calm. Anxiety can be very distressing to watch and high levels of anxiety come down naturally with time. Holding the space whilst your loved one sits with these uncomfortable feelings is difficult and often just being present is comfort in itself to them
- If your loved one is experiencing other mental health disorders, they can be addressed with their GP and may be prescribed anti-depressants or other medications. They may need support or gentle guidance to seek extra medical advice, ‘I can see you are so anxious. I wonder if you saw the GP they may be able to give you some support’
- Don’t get caught out with the reassurance trap if your loved one has anxiety
- Get out in nature - beneficial and within 20 minutes of being in nature stress hormone levels come down. Sit under a lovely tree or take a walk in a wood
Anything else?
Keep yourself well. Supporting someone with an eating disorder is a marathon not a sprint. Give yourself time out.
If your loved one is experiencing a crisis, ring NHS 111 and press option 2 (only in Peterborough and Cambridgeshire) to speak to the mental health First Response Service.
More Ideas
For information on mental health support services click here.
Our loved one is using/taking a substance, like alcohol or drugs, more then they usually would – what should we do? +
Scenario
Mental health illnesses can sometimes go hand in hand with other challenges like alcohol consumption, drug taking or addictions. This is not a given, however it is common. Drinking more alcohol then usual or taking substances may be a way of your loved one coping with something they are experiencing.
What can we do to help?
You could speak to your loved one about your concerns. Try not to judge them or be hard on them about this. Work on understanding what is going on for them to maybe they can share why they are drinking or taking a substance.
Anything else?
You can signpost your loved one to a support service. Change Grow Live (CGL) are the leading drug and alcohol support service for Cambridgeshire and are called Aspire in Peterborough. For CGL Cambridgeshire’s services follow this link.
For Aspire Peterborough follow this link.
More ideas
The SUN Network have video addiction recovery stories from individuals in recovery from addictions including eating disorders. You can watch their videos here on addiction here and their videos on eating disorders here.
The National Eating Disorders Association (NEDA) have information on this available here.
What should we do if our loved one is over-exercising? +
Scenario
Typically exercise brings physical and mental benefits. Excessive exercise causes physical and/or mental harm. Many people with an eating disorder use excessive exercise as a way of controlling weight / feelings / body shape. This can place them in physical danger. As carers we cannot make our loved ones stop exercising, although we can support them.
What can we do to help?
- If our loved one cannot contemplate changing their exercise regime, we can work towards creating an awareness of the problem. Ask yourself what the costs for them are so that you can feedback to them, e.g. are they very tired, or in pain. You can try to share observations in a calm moment, e.g. ‘I’ve noticed that you are very tired’.
- If they are receptive to change, at least to some extent, we can create ambivalence, e.g. ’On the one hand you want to go running and on the other you’ve not got enough energy to do as well as you would like to’. Use open questions ‘Why is exercise so important to you?’.
If they are serious about change, you can be more directly involved if they want you to. Remember to validate their feelings, e.g. ‘I see that this is very hard for you, I'm here for you’
Anything else?
- Relapse - if your loved one returns to over-exercising help them to get back on track by reminding them of their past successes and that you are there to support them
More ideas
See the information about compulsive exercise here.
Carers support group summary, 29th December 2020, page no: 80.
How can we help make our loved one’s transition to university a success? +
Scenario
Our loved one wants to go to university / college in a different region away from home and their support network. Possibly going against professional advice.
This is a big change that makes us and our loved one anxious.
What can we do to help?
Try to find out and understand their thoughts and feelings. They may be in two minds about going. It can be helpful to use conversations to explore the discrepancy:
‘On the one hand you really want to start your course, and on the other you are worried that you might not have the energy for a full day’s study or be able to join in with the other students’.
Let the thought sit with them. Let them draw their own conclusions.
The team supporting your loved one, the place of work, the college - all want to put measures in place so that things go well. They should welcome any information you can provide that will support them in this goal, and although this is better done with your loved one’s consent it could be done in confidence.
Plan ahead with your loved one in low stress moments, for example, having a routine, registering with a GP.
Make your own plans in advance. For example, how will you react if the move to university fails (answer calmly and learn from it!); how are you going to keep in touch (weekly call, facetime, email, text).
Anything else?
- Our loved ones have to learn to manage their illness themselves; they have to take their own decisions, even if it is against professional advice. Experienced carers have shared that loved ones were failing at university initially, but succeeding subsequently, often on a different course and/or at a different university, or apprenticeship
- Listen to their hopes and concerns; validate their worries, don't try to fix them; encourage them to think about how they have coped with this and/or other anxiety provoking situations before; help them to find their own way forward
- More validation - most people find making friends in a new place an anxious time - hearing from you, for example, that most people feel anxious when they join a club or society but this will pass, and is a good way to get to make new friends, may be very helpful
- Offer support from a distance. To quote Janet Treasure, 'They alone can do it, but they can't do it alone’
More ideas
It can be helpful to explore the range of support services available to students with your loved one, including:
- Out of hours care
- Phone lines
- Counselling, both academic and pastoral support.
All this information can be found out on the university websites.
Mental health matters - A national charity delivering mental health and social care services.
Student Minds - The UK’s student mental health charity.
The Mix - The UK’s leading support service for young people.
Carers support group summary, 14th July 2020, page no: 46, 15th September 2020, page no: 84 and 22nd September 2020, page no: 87.
How do we cope with family celebrations; Birthdays, Weddings, Religious holidays etc? +
Scenario
There is a big family birthday coming up, with visitors, lots of food and drink, changes to routines and lots of socialising.
Some of the thoughts running through your head may be:
- What can you feed your loved one?
- How can you support your loved one?
- How can you cope with critical relatives?
- How can you make sure the event is enjoyable for all family members?
Remember; family celebrations are a challenge for you, the family and of course your loved one experiencing an eating disorder. It can be very stressful for everyone
What can we do to help?
Plan!
Use a problem-solving framework to define the problem, think of ideas to solve the problem creatively and then list the pros and cons for each solution. Pick the best idea and plan it (and add a few backups).
Ask everyone what they would like to do on this occasion; pay attention to any sibling’s thoughts. Try to include some of these ideas. Discuss and negotiate with your loved one how they would like to manage the event. For example, if planning a sit-down meal having the chair nearest the door so they can leave if it gets too much without causing a physical disruption.
Prepare relatives in advance. Perhaps suggest and prepare some ‘What to say’ ‘What not to say’ ideas.
Organise some non-food activities.
Take some time out for yourself.
Anything else?
Plan!
Have a back-up plan … or two.
Be prepared to be flexible.
Try to bring some humour into the event; for example, play ‘Disaster bingo’ – think of all the things that could go wrong / be said … and then tick them off as the day progresses.
Review how it went; consider the good and bad and remember them for next time.
More ideas
Delegate some tasks to others to share the burden.
BEAT Guide for friends and family.
Carers support group summary, 8th December 2020, page no: 70.
How can we help our loved one cope with Christmas? +
Scenario
Christmas can be a particularly stressful time for people with eating disorders. It’s not just that the celebration centres so much on food and drink but also that it is a big social occasion with all the anxieties that brings, e.g. friends and family might not know how things are, and what to say. For parents and carers, we want to help our loved ones as much as possible and we also need to manage our own stress levels that would probably be high even under normal circumstances.
What can we do to help?
Fortunately, there is a lot we can do to help. A good way forward is to take an inclusive problem-solving approach. ‘Flip’ your mindset to ask, ‘How can we make Christmas good for everyone, including ourselves?’, rather than just asking, ‘How can we make Christmas good for our loved one?’ The following ideas came out of a support group discussion in December 2020.
Ask everyone 'What is the one thing you'd like to do this Christmas?'
Everyone suggests the food they want to eat.
Discuss / negotiate with your loved one how they are going to manage the meal itself, e.g. having the chair nearest the door so that they can leave if it gets too much without causing a physical disruption.
Organise a few non-food activities you can do together as a family - board games, films, charades, Desert Island Discs. Similarly, play some party games not to do with food.
Christmas 'disaster bingo' - think about all the things that could go wrong / be said… and then tick them off as the day progresses. (Editor's note: this seemed to be alarmingly popular!)
Plan the day carefully, with timings.
Prepare grandparents, aunts/uncles, friends/family in advance.
Ask siblings what they are worried about/what you can do to help, do not make assumptions; and involve then in the preparations/activities.
Have contingency plans(plural).
Include a walk as part of the plan.
Play some music together!
Anything else?
List the pros and cons of each of the ideas, e.g. for 'What is the one thing you'd like to do this Christmas?' Advantage: everyone will feel that they've had a chance to have their say and therefore have a stake in the occasion. Disadvantage: some of the ideas might not be feasible, or might be incompatible, leading to disappointment.
Having worked through all of the ideas it will then be possible to give them a score out of ten so that you can rank them and draw up a list of the top three or four things to do.
More Ideas?
With siblings it is important to listen to their concerns / worries and to validate these - it is rotten for them and that is a perfectly normal reaction, they should not feel guilty about it. Unless you know what they are thinking and feeling you are flying blind and they won't feel that their views are being taken into account.
If your loved one is in an inpatient unit over Christmas and will therefore not be with you, it is not going to feel the same as usual and this has to be acknowledged. On the other hand, it is an opportunity to look after yourselves, to relax the best you can, and not feel guilty.
If it gets too much, have a bit of time out and then come back. To misquote Shakespeare, although I'm sure it's what he intended to say, 'Exit, as would a dolphin', i.e. calmly swim out of view for a few moments!
To help friends and family understand eating disorders better, send them a copy of BEAT’s guidance for friends and family.
(And remember, ‘All Things Must Pass’. At the end of the day, it’s no longer, or shorter, than any other day.)
Our loved one finds it difficult to food shop for themselves/decide what to buy - How can we best help them? +
Scenario
This is a common question. Our loved one can be anxious about one or more of a number of things, e.g. calorie content, not wanting to be seen carrying a large grocery shop, not buying the food they would like because they feel they do not deserve it, being overwhelmed by the sheer choice available.
What can we do to help?
- Writing a shopping list as part of menu planning - the ideas for meals could come from a range of sources, e.g. online recipes that list ingredients.
- Going to smaller shops / supermarkets where the choice is less than at large ones.
- Reducing the amount of choice if you are shopping with them, but not taking the final decision, e.g. 'You decide between these two, I am happy with either'.
- Shopping at quieter times of the day.
Anything else?
The ability to food shop independently is very much a part of the recovery process and generally improves alongside other gains in our loved one's health.
More Ideas?
Meal-kit companies, e.g. 'Hello Fresh' and ‘Simply Cook’ offer meal boxes where you choose meals online and the ingredients are delivered to your door, with cooking instructions. Carers have reported that these have helped their loved ones. They have to choose the meals and are responsible for their preparation, so they are fully involved, but they do not have the potential stress of shopping for a lot of different ingredients. They can progress to buying their own ingredients for the recipe cards.
There are foods our loved one really enjoys but they just can't bring themselves to buy and/or eat them - how can I help? +
Scenario
This is a very common issue. It is a positive sign that our loved one wants to change their behaviour, but how best to help them?
What can we do to help?
- In a low stress moment, discuss the support your loved one would like. Ask what is helpful and unhelpful to say or do. Be prepared for the first response to be ‘nothing’. Let it hang. Very often they will return to the conversation later.
- If your loved one is making a change, e.g. introducing a food that they would like to eat but find difficult, organise ‘wrap around care’. This means, ideally, having a calming activity prior to the meal and something they really like doing planned for after the meal.
- ‘Nudge’ the conversation in a calm moment, e.g. ‘I’ve noticed that you no longer have pizza but you used to really like that’. Be prepared to leave the question hanging - do not insist on a response.
Anything else?
Some carers have reported that ‘food challenge jars’ have been helpful: your loved one writes the foods they would like to eat, one each on a piece of paper, pops them in a jar and pulls out one or two a week to re-introduce into their diet.
More Ideas?
BEAT has suggested ‘Mindful Eating: A guide to rediscovering a healthy and joyful relationship with food’ - By Jan Chozen Bays.
We are worried that our loved one might be slipping backwards but they do not talk to us about their weight, or monitoring results - what can we do? +
Scenario
Many of us have faced this situation. In Cambridgeshire and Peterborough blood results for patients monitored by the service are always checked by a medical specialist. If there is any cause for concern, e.g. an aspect of blood chemistry that is significantly abnormal, the patient will be contacted - this is important reassurance for us as carers.
What can we do to help?
- Practice varies around the country, so this is something you should ask your loved one about and encourage them to ask if they do not know.
- Confidentiality means that even if you were to ask for their medical monitoring information it would not be provided and trying to find out behind your loved one’s back would unnecessarily risk your relationship, so this is something to avoid doing.
- It is important not to ignore the issue - this will send the wrong message to your loved one, i.e. ‘They’ve not said anything, so I must be alright’. Find a calm moment to be brave and gently offer an observation, e.g. ‘You’re probably not going to like me saying this but I’ve noticed that….. Perhaps there is something I can do to help?’
Anything else?
Carers have reported some interesting and original ways to work with their loved ones, e.g. entering results on a shared spreadsheet, or a weekly weigh-in on Zoom if they are living away from home.
The SUN Network has put together a leaflet about medical monitoring with eating disorders, which you can read and download here.
More Ideas?
It is helpful to understand that recovery is rarely linear and ‘lapses’ are common. Treat these as part of recovery, this link has some useful information.
Our loved one struggles when their routine changes: how can we help? +
Scenario
Carers often talk about their loved ones struggling when their routine changes, e.g. at the weekend, or at the end of term. It is perhaps not surprising that 'forced' breaks like these are difficult. Suddenly our loved ones are faced with a period with nothing organised for them and there is a risk they start dwelling on their eating disorder or get anxious because 'they are not doing anything'. Research has consistently shown that routines help people manage stress and anxiety because they give structure and control.
What can we do to help?
- As carers we can encourage our loved ones to plan an alternative routine that includes activities they enjoy and will give a sense of achievement, however small.
- 'Activity scheduling' can help, e.g. putting together a plan for the day that includes some ‘necessary’ activities, such as the laundry, with ‘pleasurable’ activities, e.g. time to pursue a hobby.
- We can also help our loved ones understand that weekends, for example, are there for a reason - people need recovery time from work. Getting up late, watching a few movies on the television and catching up with some friends on the phone is normal and necessary.
- Validate: 'I'm not surprised you're exhausted after the week you've had'; 'It was a really good idea to watch the rugby on the television this afternoon, my guess is you feel less tired for that'.
- Also… model good practice!
Anything else?
It's really good to have non-eating disorder interests to talk about and engage with and 'downtime' can be a good time for these, e.g. a football match, a museum trip. These can be planned into days off, giving structure and something else to talk about.
More Ideas?
This website has some interesting and useful ideas about routines and how to establish them, which could be adapted to different circumstances.
How do we help our loved ones when they 'want to do more' but can't bring themselves to do it? +
Scenario
This is a common scenario in the early stages of recovery when our loved one is contemplating change. This is positive, but for carers it can be very frustrating because what they should be doing seems so obvious and straightforward. However, it is important not to step in and take over because this is likely to result in resistance. Our loved ones may well be scared of what they are going to lose, e.g. being protected from their emotions, or being cared for. It is important to take time to understand our loved one’s anxieties so that we can best support them.
What can we do to help?
- Whenever they want to talk, seize the moment. Be curious, ask open ended questions, ask how you could help and try to find out what they fear… but stay calm and don't be overbearing.
- Help them find their motivation. Something worth getting well for' is a powerful spur for recovery. One way to do this is to explore 'pros' and 'cons', e.g. 'On the one hand you want to be a bridesmaid at your sister's wedding and on the other you are worried about the costume fitting and whether you will have enough energy for the big day'. Let it hang, there is no need for an answer or response, it is all about helping them clarify their thoughts.
- Make connections between their eating disorder and its consequences on their health, behaviour, and activity. Present these in a factual, not a judgmental, way, e.g. 'If a person hasn't had enough to eat it is difficult for them to concentrate' rather than 'You can't concentrate because you don't eat enough'.
Anything else?
Discuss possible plans of action, i.e. what they could do. If you're anything like me you'll be desperate for your son or daughter to agree to x, y and z and sign on the dotted line, but it is essential that the decision is theirs, and in their own time. It really is a moment to stay calm and patient.
More Ideas?
Read about the Change Cycle on BEAT’s website here.
Our loved one is having trouble sleeping, is there anything we can do to help? +
Scenario
This is a common question because an eating disorder (lack of food, too much food) affect sleeping patterns. It can cause our loved one’s great distress and make it more difficult for them to think clearly and to have the energy they need at the right times of the day, e.g. when they have a treatment session.
What can we do to help?
- Carers have reported that their loved ones have found weighted blankets helpful to reduce stress and improve sleep. A google search will show you many possible suppliers, for example calming blankets. Weighted animals perform a similar function, which you can read more about here.
- The NHS has some very useful advice here.
- Not napping during the day, a regular bedtime and getting up time and avoiding caffeine after midday were also mentioned as having been helpful.
Anything else?
There are many apps that offer guided self-help to reduce anxiety and improve sleep. For example, the CALM app was recommended at a Cambridgeshire and Peterborough Carers Support Group.
More Ideas?
Read the Sleep Hygiene leaflet produced by the Centre for Clinical Interventions in Australia, which covers 15 tips for better sleep here.
How can you help family members (and yourself) to not feel blame or guilt? +
Scenario
It is very common when people have an eating disorder that parents/carers/family members feel they are to blame for their loved one’s illness, but there is no evidence that this is the case. Eating disorders are a complex mental illness; many factors contribute to eating disorders like genetics, brain structure, cultural elements, reactions to trauma and biology. Parents/carers/family members can also feel guilt for things that they do, e.g. going out for a meal with their partner, not driving another two miles to buy the 'perfect food', going to a concert without their brother or sister. This feeling of guilt can become overwhelming.
What can we do to help?
If it is someone you are trying to support:
- Validate – Say to the person who is feeling blame or guilt, 'It's absolutely understandable that you feel like that, it's perfectly normal for parents/carers/family members to feel a responsibility for their loved one's health'.
- Talk - ask open questions to explore their feelings.
- Reflect - say what you think you have heard, to help them make sense of their thoughts, and to check your understanding.
- Affirm - praise something that they have said or done that will develop their self-confidence, e.g. being brave, or honest, or open.
If it’s you… practice self-compassion:
- Take breaks, pause.
- Pay attention to your thoughts and feelings, don't ignore them.
- Find your strategy for creating some 'headspace', e.g. mindful breathing, visualising your ‘safe/favourite’ place.
- Look after yourself.
Anything else?
Remember - it is normal to feel guilt and it is important to allow people to have feelings - success is helping them to express these feelings, not fix them.
More Ideas?
Here are details of two books on self-compassion that have been recommended by a local carers support group. The first book: ‘Self- Compassion' by Kristen Neff (paperback, hardback, Audible, Kindle) is aimed at everyone, the second: 'Fierce Self-Compassion' by Kristen Neff (hardback, Audible, Kindle & paperback from 7 July 2022) at women.
People are avoiding us, and my social support network is collapsing - what can I do? +
Scenario
This is, unfortunately, a common scenario - people, including close friends and family, stop inviting you to social occasions. They start leaving you out because they don't know how to react to you / your loved one, and/or what to say. This makes a difficult situation worse because a social support network is important to anyone’s resilience. Now is the very time when you want as many people on your team as possible, helping as much as they can.
What can we do to help?
- Ideally, you need to sit down with some key friends and family members and explain how you are feeling, what you understand about eating disorders and how they can best help you and your loved one. This is not always possible but there is some very good information that you can give friends and family, e.g. BEAT's ‘Guide for Friends and Family', which you can encourage them to read.
- FEAST’s ‘A Guide for Family and Friends’ has a very interesting list of twenty suggestions for how friends and family can help
Anything Else?
There will always be some people who 'don't get it' and will say the wrong thing, e.g. the aunt or uncle who says, 'Wow, you're looking better, you've put on so much weight'….. This is so predictable that it is something that you should discuss in advance with your loved one, in a calm moment, so that they (and you) can prepare your reaction – it’s part of the process of developing resilience. This will help social occasions go better.
More Ideas?
A close family member is critical of your approach and/or the treatment your loved one is receiving and its causing worry and upset, for you and your loved one – what can you do? +
Scenario
This scenario has been raised several times at support group meetings. It could be your former partner, your mother, your father-in-law – they are not as involved as you are, but they think you are doing it wrong and that their ideas are better. The trouble is, they really don’t understand what an eating disorder is, or what you are having to do.
What can we do to help?
- You might not want to, but it is important to validate their concern – it is good that they are taking an interest, it means they are a potential source of support. Experience suggests that they will be more likely to listen to you and you can do this without agreeing with their suggestions.
- Avoid ‘but’, use ‘and’. This makes the conversation less confrontational, and it makes you more proactive and less reactive. For example, ‘I really appreciate that you want to help, and it would be great if you would xxxxx’.
- It's important to be assertive (rather than passive, or aggressive) - be clear and open about what you think and feel without being blamey or critical of the other person. It may be necessary to put some boundaries in place if they are needed.
- If the conflict is unsettling your loved one, give them opportunities to talk about it, and be honest about how you feel.
Anything Else?
- Don't feel guilty. It's not your fault. You are not responsible for what other people think. If you are being blamed for your loved one’s illness, remember that an eating disorder is a complex mental health illness and there is no evidence that eating disorders are caused by parents and carers. Perhaps the other person does not know or understand this. Carers have reported that something as simple as providing BEAT's Friends and Families booklet has been helpful.
- Get support for yourself if you need it. Caring for a loved one with an eating disorder is stressful enough as it is, and there is only so much anyone can cope with by themselves.
More Ideas?
If you google ‘what not to say to someone with an eating disorder’, you will get a lot of results. This site has a useful list, and it also says what you should say and do. It could be an eye-opener for someone who thinks you are doing things wrong.
Should people with an eating disorder go on holiday to a destination where there could be some health risks, e.g. from contaminated water or food? +
Scenario
Although a holiday abroad can be very challenging for someone with an eating disorder because it takes them away from their support network and routines, at a point in their recovery it can be very motivating. The question in this FAQ came up in relation to a family holiday that had been planned before their loved one became ill but it could apply to travel to any region where visitors are advised to take extra precautions and/or have specific vaccinations / take medication such as malaria tablets. The concern, of course, is avoiding unnecessary risks, e.g. our loved one getting a stomach bug when they are already underweight.
What can we do to help?
- What are the medical risks? It’s important that you and/or your loved one have a discussion with their clinician, or GP.
- What does your love one think about it? If it’s a family holiday, you don't want them to think that they are the reason for you not going, so there needs to be some sensitive discussion. Their motivation is vital and if there is a medical risk, you can appeal to the higher authority, i.e. 'the doctor said… it's not you or me'.
- If it’s a family holiday, what do you and the rest of the family think? If you are going to be too worried to enjoy it you are almost certainly setting things up for failure, but this is something that you would have to explain to your loved one.
- Ask yourself 'What is the worst thing that could happen?' You may well feel that you/they could plan to deal with this.
- Reduce risk by drinking bottled water, maintaining good hand hygiene, being careful about where you eat, avoiding food that you are not sure of, avoiding meat, take medication for upset stomachs.
Anything Else?
-
Could you/they go somewhere else equally exciting but less 'risky'? And whatever you/they decide, be honest with the travel insurance company, unless you can meet the financial risk of medical bills yourself; specialist insurance is available.
More Ideas?
There is an interesting account, related to this question, on the BEAT website https://www.beateatingdisorders.org.uk/your-stories/travelling-overseas-eating-disorder/ .
The community team are recommending our loved one is admitted to an inpatient unit: should we be worried about this? +
Scenario
Most people with an eating disorder are treated as outpatients. The decision to offer inpatient treatment is based on a range of indicators that mean our loved one’s health cannot be managed safely in the community. These include physical factors, e.g. rate of weight of loss, abnormal blood results, blood pressure, core temperature and strength tests, as well as psychological factors, i.e. our loved one’s state of mind. You shouldn’t be worried about inpatient treatment, although your concern about your loved one’s health is understandable. As carers we should be reassured that our loved one is getting appropriate, specialist care.
What can we do to help?
- Inpatient treatment has advantages and disadvantages for our loved one, e.g. it is more intensive, but it is more disruptive of normal life. You could offer to help with some of the practicalities, e.g. pet care, keeping an eye on the flat.
- As carers we should take the opportunity of a reduced caring responsibility to recharge our batteries: this is important.
- Being worried about our loved one’s return home is quite understandable. However, this will be a managed (usually staged) process. We are never left on our own without a number to ring. There is always a discharge plan, and this will involve us as carers unless there are exceptional circumstances.
- Inpatient admission can have practical implications for us as carers, e.g. time out of work / additional expenses in order to attend meetings / visit. The inpatient unit can arrange a formal Carers Assessment for you that may be able to provide support, including financial help and respite care.
Anything Else?
- Inpatient treatment is not a quick fix. It is part of a process of recovery that can take a long time. It’s important that we manage our expectations.
- Some patients are unable to maintain their health on discharge and require a second admission. This is a very worrying time for carers. It is important to remember that most people do recover, recovery can take a long time and it is a roller coaster with ups and downs. Therefore, it is important that we look after ourselves.
More Ideas?
The inpatient unit that will be treating your loved one will have information for carers, and service users, so do ask for this if it hasn’t already been provided. This link contains some useful information, as does the rest of the site, which was advised by some respected names in eating disorders provision in this country https://healthtalk.org/eating-disorders/staying-in-hospital.
I worry about my loved one's health, but I don't know what to say because I've said it all before: what can I do? +
Scenario
Recovery from an eating disorder can be a long, slow process. Especially in the early days of the illness, when the ‘eating disorder voice’ is at its strongest, progress can be very slow. Understandably, this is an intensely worrying time for carers, and it can feel as if our support and advice is falling on deaf ears. This can lead to frustration, which can boil over into anger and upset. However, there are things we as carers can do, although it will be necessary to think about the eating disorder a little differently.
What can we do to help?
- Don't feel compelled to say something. Success is helping our loved ones to express their feelings; it's not fixing their problems. They may not want us to say anything – be there, be present – that in itself is really hard work.
- Ask rather than say, e.g. 'There is no need to answer straight away, have a think, and let me know what I could do to help’.
- Validate their concerns and affirm any positive actions they are taking, however small, e.g. 'I'm not surprised you're finding meals difficult now that you’re home, it's different to being in hospital, and I am really impressed with your determination'.
- Try to talk about something not to do with the eating disorder.
Anything Else?
If this is the scenario you are facing it is highly likely that your loved one is in either the ‘pre-contemplation’, or the ‘contemplation’ stages of the Change Cycle. Some things we can do as carers in addition to the ideas already mentioned include:
- Providing factual, non-judgemental, feedback about their health, e.g. ‘I can see that you’ve lost weight’, rather than ‘I’m really disappointed that you’ve lost weight again, it’s because you’ve not been sticking to your meal plan’.
- Discuss the pros and cons of change, e.g. ‘On the one hand you want to join your friends on holiday and on the other hand you’re too tired because your body is lacking the energy it needs’. There is no need to follow up this statement, leave your loved one to work out their own conclusion.
- If they do show a desire to start changing their behaviour, discuss possible action plans, but don’t jump ahead and begin detailed planning, i.e. ‘what could you do?’ rather than ‘what will you do?’
- And don’t forget to look after yourself – exhausting yourself will mean that you are less able to help when your loved one is ready for change.
More Ideas?
Have a look at the FAQ on this website ‘Our loved one is stuck - how can we help motivate them to make the next step in their recovery? It has some ideas that might be relevant to this scenario. It also mentions these two resources about the Change Cycle:
- Motivational interviewing, see pages 94-99 of Skills-based Caring for a Loved One with an Eating Disorder by Janet Treasure, Grainne Smith and Anna Crane. Routledge. ISBN 978-1-138-82663-2. 2nd edition.
- Eating Disorders: Stages of Change Video
Other helpful links to further information +
Services information
 PEDS - Personalised Eating Disorder Service is a charity based in Peterborough, who offer support to people experiencing eating challenges.
PEDS - Personalised Eating Disorder Service is a charity based in Peterborough, who offer support to people experiencing eating challenges.
 Cambridgeshire and Peterborough Foundation Trust for Carers (NHS) - This is the local branch of the NHS for Cambridgeshire and Peterborough who offer support for carers. Some of the services CPFT provide for carers are if your loved one is currently accessing support and others are if your loved one has been referred into services.
Cambridgeshire and Peterborough Foundation Trust for Carers (NHS) - This is the local branch of the NHS for Cambridgeshire and Peterborough who offer support for carers. Some of the services CPFT provide for carers are if your loved one is currently accessing support and others are if your loved one has been referred into services.
CPFT's Keeping Safe Programme - The Keeping Safe programme is the first step in treatment. It has been developed to provide information to help you begin to make sense of your difficulties and to encourage you to take steps to minimise any potentially harmful effects caused by your eating disorder whilst you are waiting for treatment. This programme also has a workbook for family and friends of those struggling with an eating disorder.
 CPSL Mind - Cambridgeshire Peterborough and South Lincs Mind are a local charity that is part of Mind’s national charity. They deliver various services to support individual’s mental wellbeing.
CPSL Mind - Cambridgeshire Peterborough and South Lincs Mind are a local charity that is part of Mind’s national charity. They deliver various services to support individual’s mental wellbeing.  Relate - Deliver counselling for people living in Cambridgeshire or Peterborough.
Relate - Deliver counselling for people living in Cambridgeshire or Peterborough.
 CGL Cambridgeshire (Change Grow Live Cambridgeshire) - are the main provider for substance addiction support in Cambridgeshire
CGL Cambridgeshire (Change Grow Live Cambridgeshire) - are the main provider for substance addiction support in Cambridgeshire
Aspire Peterborough - is part of Change Grow Live (CGL) who provides substance addiction support in Peterborough.
 First Response Service Mental health crisis support NHS 111 option 2, 24-hour support service for people in Cambridgeshire and Peterborough. Upon calling you speak to trained mental health staff.
First Response Service Mental health crisis support NHS 111 option 2, 24-hour support service for people in Cambridgeshire and Peterborough. Upon calling you speak to trained mental health staff.
 Rethink Carers Support - Advice and support for those caring for someone with a mental health illness and those experiencing a mental health illness. You can view the Cambridgeshire and Peterborough Rethinks here. You can view their carers information hub here.
Rethink Carers Support - Advice and support for those caring for someone with a mental health illness and those experiencing a mental health illness. You can view the Cambridgeshire and Peterborough Rethinks here. You can view their carers information hub here.
 CPFT Eating Disorders Online Carers Support Group - When the country went into lockdown, CPFT arranged to replace the monthly Eating Disorder Carers Support Group with a weekly online meeting to provide support and advice. You can read their previous summaries here : Book 1, Book 2, Book 3 and Book 4.
CPFT Eating Disorders Online Carers Support Group - When the country went into lockdown, CPFT arranged to replace the monthly Eating Disorder Carers Support Group with a weekly online meeting to provide support and advice. You can read their previous summaries here : Book 1, Book 2, Book 3 and Book 4.
Carers Direct Helpline - If you are a carer, the helpline advisers can give you information to help make decisions about your personal support needs and the needs of the person you're looking after. This information includes assessments, benefits, direct payments, individual budgets, time off and maintaining, leaving or going back to work or education. The Carers Direct helpline doesn't however; provide personal financial, medical or legal advice and doesn't provide casework, advocacy, representation or counselling.
 Carers Trust - We work to improve support, services and recognition for anyone living with the challenges of caring, unpaid, for a family member or friend who is ill, frail, disabled or has mental health or addiction problems. We do this with a UK wide network of quality assured independent partners and through the provision of grants to help carers get the extra help they need to live their own lives.
Carers Trust - We work to improve support, services and recognition for anyone living with the challenges of caring, unpaid, for a family member or friend who is ill, frail, disabled or has mental health or addiction problems. We do this with a UK wide network of quality assured independent partners and through the provision of grants to help carers get the extra help they need to live their own lives. Making Space - We provide services in the heart of local communities, in the comfort of people’s own homes, and specialist care and support services. Our professional, caring employees and volunteers deliver our services with dignity, respect and compassion, focusing on outcomes that help the people we support have the freedom to enjoy an everyday life.
Making Space - We provide services in the heart of local communities, in the comfort of people’s own homes, and specialist care and support services. Our professional, caring employees and volunteers deliver our services with dignity, respect and compassion, focusing on outcomes that help the people we support have the freedom to enjoy an everyday life. PinPoint - Helping Cambridgeshire parents who have children with additional needs and disabilities. Pinpoint Cambridgeshire is run for parents – by parents. We give help and information to parent carers of children and young people aged 0-25 with additional needs and disabilities, and give parent carers opportunities to have a say and get involved in improving local services.
PinPoint - Helping Cambridgeshire parents who have children with additional needs and disabilities. Pinpoint Cambridgeshire is run for parents – by parents. We give help and information to parent carers of children and young people aged 0-25 with additional needs and disabilities, and give parent carers opportunities to have a say and get involved in improving local services.

Caring Together’s vision is a world with no unpaid carer in crisis, isolated or struggling alone. If you are an unpaid carer, they are there to help you. They can give you information and advice, and provide services and support to make your caring role more manageable, to benefit you and the person you support. Calling them on 0345 241 0954, email hello@caringtogether.org or visit caringtogether.org
 Mental Health Matters - A national charity delivering mental health and social care services.
Mental Health Matters - A national charity delivering mental health and social care services.
 Student Minds - The UK’s student mental health charity.
Student Minds - The UK’s student mental health charity.
 The Mix - The UK’s leading support service for young people.
The Mix - The UK’s leading support service for young people.
 Nightline - a listening, emotional support, information and supplies service, run by students for students.
Nightline - a listening, emotional support, information and supplies service, run by students for students.
Resources
Leaflets
Books
The below books/authors were recommended by those with lived experience of eating disorders:
- Hope Virgo
- Emma scrivener
- Jenny Langley
- Tina McGuff
- The Invisible Man - A Self-help Guide for Men With Eating Disorders, Compulsive Exercise and Bigorexia
- Samuel Pollen - author of The Year I Didn’t Eat
- Christopher Eccleston - I Love the Bones of You
- Rhik Samadder - I Never Said I Loved You
- Andrew Walen - Man Up to Eating Disorders
- MaleVoiced - this website is specifically for male ED suffers and has some brilliant resources including this great list of books
- Beat have suggested books
- Mindful Eating: A guide to rediscovering a healthy and joyful relationship with food - By Jan Chozen Bays
- Life without ED by Jenni Schaefer
- 8 keys to recovery by Geneen Roth
- The Inside Scoop on eating disorder recovery: Advice from two therapists who have been there by Colleen Reichmann and Jennifer Rollin
- Goodbye ED, Hello Me: Recover from your eating disorder and fall in love with life by Jenni Schaefer
- Body Image Workbook
- The secret language of eating disorders, Peggy Claude-Pierre
- The War of art - Steven Pressfield
- Sick enough: A guide to the medical complications of eating disorders by Jennifer L Gaudiani
- Thinsanity by Glen Mackintosh

Websites

Videos

Podcasts
